For those of you who don't know what IVF is, I've documented this below. I've captured "my version" and the medical version.
There's even a cool virtual tour here.
My version:
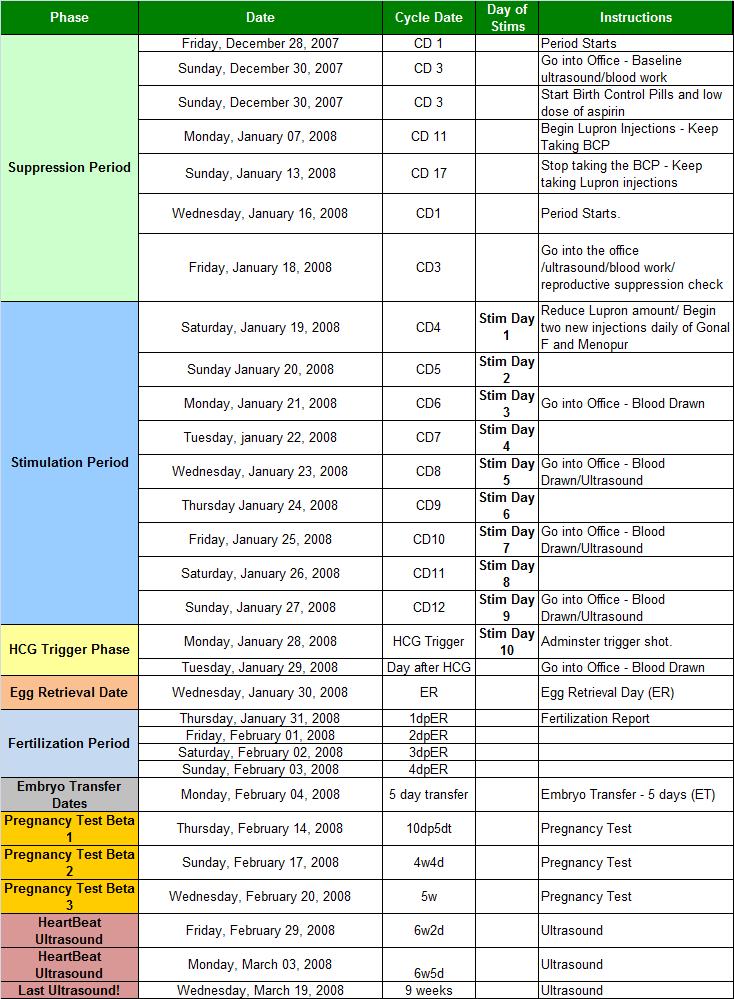
- They first run me through many diagnostic procedures to ensure my uterus and 'girl bits' are working as they should. Two of these procedures are called SHG and HSG. I've heard these aren't the most pleasant things in the world, but are neccessary to make sure my bits are in fine working order. They are very specific about when these tests can take place, the vaginal ultrasound needs to be 3 days after my period. The other two need to be 5-12 days after my period and so on and so on.
- Then they put me on fake hormones - birth control pills - to "suppress" my natural reproductive system. They basically wanna be in charge, they wanna run the show.
- Then more hormones - these are hormones I will inject myself with every day - to stimulate the shit out of my ovaries in order to get as many egg follicles growing as possible.
- They will monitor me often - checking to see how my follicles are doing, whether or not they are getting to the "ripe" old age of maturation.
- When they're ready, they suck those little puppies out. I hope to get 15-20+ eggs. Women normally produce ONE a menstrual cycle. :o
- The day of my "egg retrieval", M has a sperm aspiration as well.
- They take one single sperm and inject it into each good quality egg. This procedure is called ICSI.
- The lab fertilizes my eggs with M's sperm. The little cells start to divide, forming what will later be known as 'baby'. They grow those little kiddos out to 3 days or 5 days depending on their quality. These are called embryos. Some survive. Some don't. Some are good 'quality', some aren't.
- For those that survive, we decide how many to transfer into my uterus. A couple days later, I go back in and those little suckers are dropped into my womb and I take it easy for a couple of days, hoping those little guys implant themseleves nice and happily.
- 8-12 days later I come back into the clinic to see if the embryos "stuck" (implanted) aka, if I'm pregnant. If so, they will monitor my HCG levels to see if there is more than one fetus in there. (!!)
- Boom bang bam, we're pregnant. But it doesn't always work. This is to be expected. If it doesn't, we do a second IVF cycle. And third and so on. Of course, this is leaving out a lot - like the injections I'll need to give myself, the emotional strain, the weird doc hands in my cooch and all the lovely things that come with vaginal scenarios.
Now for the Medical Version:
IVF Process
The following text outlines our process for an IVF cycle:
Suppression of the reproductive hormone system: We must suppress the natural hormones in order to allow multiple follicles to develop (normally, only one develops) and to prevent spontaneous ovulation of the oocytes before we can retrieve them for our purposes. We use several medications such as oral contraceptive pills (OCP), Lupron (GnRH agonist), Antagon or Cetrotide (GnRH antagonists) in various combinations to achieve suppression.
Stimulation of the ovaries: We use gonadotropins (FSH, LH) in high doses to stimulate the ovaries to produce a large number of oocytes. Women differ widely in the number of oocytes their ovaries will produce but we hope to retrieve between 5 and 20 oocytes with each stimulation cycle. We monitor the progress of the stimulation with blood hormone levels and vaginal ultrasound measurements of the ovarian follicles.
Retrieval of the oocytes: We plan for retrieval of the oocytes when the hormone information and follicle size indicate that the oocytes are mature and ready for fertilization. Our staff instructs our patients to administer the hormone HCG about 35 hours before the planned retrieval. This initiates the final steps of oocyte maturation and allows the oocytes to be removed from their follicles. With the woman under conscious sedation and using ultrasound for guidance, we pass a fine needle through the vaginal wall into each of the ovarian follicles and aspirate its contents. The fluid obtained from the follicles is transferred directly to the IVF laboratory where the embryologist identifies the oocytes under the microscope and places each one into its own dish containing special culture medium.
Fertilization of the oocytes: Usually, while the ovum retrieval is underway, the woman’s partner provides a semen sample from which we isolate sperm to fertilize the oocytes. Other possible sources include sperm obtained previously and frozen, donor sperm from a sperm bank and sperm obtained through aspiration of the testis for men with obstructive azoospermia. The sperm sample is prepared in the andrology laboratory (see below for details and variations) before being added to the dishes containing oocytes. The oocytes and sperm incubate overnight to allow fertilization to take place. In cases where impaired fertilizing ability is suspected, we directly inject a sperm into the oocyte to achieve fertilization (ICSI). Successful fertilization is determined the next day by locating two nuclei within the oocyte ("2PN stage"). The fertilized oocyte is now called a zygote.
Embryo Development: Each zygote is placed into fresh medium and incubated further to allow cell division to occur. Once cell division begins, the zygote is now called an embryo. The embryonic cells ("blastomeres") remain contained within the egg’s outer coating, called the "zona". By the 3 rd day after retrieval, most embryos will have reached the 8-10 cell stage and may be ready for transfer. After another 2-3 days, the embryo has more than 100 cells and is called a "blastocyst".
Embryo Transfer: Selected embryos are returned to the uterus through a procedure called an "embryo transfer". This is a painless procedure involving the introduction of a thin tube (catheter) into the uterine cavity through the cervix. The embryos are passed from the catheter into the uterus where implantation takes place. The embryologist guides us in selecting a limited number of the best embryos for transfer. Selection criteria for embryo transfer are designed to maximize pregnancy rates and minimize multiple pregnancy rates. Whenever possible, we freeze the remaining embryos for future use. The number of embryos to transfer is determined by the anticipated implantation rate. Implantation rate refers to the number of implanted embryos per total number embryos transferred as determined by the number of gestational sacs visible by ultrasound 4 weeks after transfer. Implantation rate is determined mainly by embryo quality which in turn depends largely on a woman’s age. Embryo quality is also dependent on the conditions within the embryology laboratory.
Luteal Phase Support: The ovary produces progesterone after natural ovulation and after IVF oocyte retrieval. However, during the course of ovum retrieval, we remove a large number of the progesterone producing cells along with the oocytes. Consequently, some women may not produce sufficient progesterone themselves to support a new pregnancy. So, we supplement all IVF cycles with additional progesterone during this critical stage. Progesterone supplements may be administered by injection or by the vaginal administration of tablets or gels.
Pregnancy Test: We test for pregnancy using a blood test about 14 days after egg retrieval. By that time, the HCG administered to trigger the retrieval should be out of the system and any HCG measured in the blood will be from a new pregnancy. Some pregnancies last only a few days ("biochemical pregnancy") but most progress to at least 6 weeks when we can see them with ultrasound ("clinical pregnancy"). It is at this point that we can determine how many embryos have implanted.